Exploring barriers and facilitators of preceptorship in undergraduate health professions education: insights from a qualitative needs assessment among preceptors in Eastern Uganda | BMC Medical Education

The findings from this needs assessment highlight the complex interplay of facilitators and barriers to effective preceptorship at Busitema University, Mbale College of Health Sciences, and Mbale Regional Referral Hospital. The findings revealed that effective preceptorship is supported by both external and internal factors, including material support from partners such as Seed Global Health, the strong commitment of clinical staff to student mentorship, and the collaborative involvement of faculty and postgraduate students. However, the effectiveness of preceptorship is significantly hindered by several systemic and logistical challenges. These include overcrowding of students in clinical settings, limited coordination between academic and clinical institutions, a lack of formal training in preceptorship among clinical staff, faculty shortages, insufficient time allocated for clinical rotations, and inadequate resources for practical skills demonstration. These results highlight the complexity of clinical education in low-resource environments and point to key areas requiring strategic investment and policy attention. These insights are very important for understanding how to optimize clinical training environments, particularly in resource-limited settings like Eastern Uganda.
Facilitators of preceptorship
Our findings revealed that support from Seed Global Health, through provision of essential medical equipment and training resources, was a critical facilitator of preceptorship. Seed Global Health is a U.S.-based non-profit organization founded in 2011 whose mission is to expand access to quality care and improve health outcomes for all through long-term partnerships with ministries of health, universities, and hospitals. Its governance structure involves collaboration with national governments and academic institutions, ensuring that interventions align with country health priorities. Funding for Seed Global Health comes from philanthropic donations, grants, and international development partners, which allows it to invest in medical education, clinical training, and capacity-building initiatives [8].
For preceptors in Mbale regional referral hospital and Busitema university, the provision of teaching aids such as flip charts, clinical equipment, and the presence of Seed educators were particularly highlighted as strengthening both teaching and learning. This aligns with previous studies that emphasize the importance of resource availability in enhancing the quality of clinical education [3]. The presence of external educators not only enhanced the knowledge base of students but also brought in diverse and friendly teaching methodologies, which are often lacking in local settings. Comparable initiatives in Sub-Saharan Africa include Partners In Health (PIH), which integrates education and service delivery across several African countries; IntraHealth International, which focuses on strengthening the health workforce through training and digital innovations; and the Medical Education Partnership Initiative (MEPI), a U.S. government funded program that has supported capacity building in medical schools across Africa [9,10,11].
Furthermore, the extrinsic and intrinsic motivation and willingness of hospital staff to engage in teaching were identified as critical facilitators of clinical education. This intrinsic motivation is consistent with previous studies demonstrating that healthcare professionals’ engagement in teaching is often driven by a sense of professional duty and the desire to contribute to the development of future practitioners [12]. Within the Busitema University teaching context, teaching is a formal component of faculty members’ academic responsibilities and is typically recognized within their institutional workload. In contrast, most hospital staff who participate in student teaching do so voluntarily, with limited formal recognition or financial compensation. Their contribution, therefore, appears to be primarily sustained by intrinsic motivation rather than by extrinsic institutional incentives.
The involvement of postgraduate students similarly played a pivotal role in maintaining preceptorship activities. While this participation aligns partially with their own learning and training requirements, it also reflects a strong culture of mentorship and professional stewardship. This model is consistent with international best practices in medical education, where the engagement of senior trainees and residents in teaching has been shown to enhance both learner outcomes and the mentors’ own professional development [13]. Collectively, these findings emphasize the importance of balancing institutional expectations with recognition and support for intrinsically motivated contributors, to ensure the sustainability and quality of clinical teaching within resource-constrained training environments.
Barriers to effective preceptorship
Despite the facilitators described above, several barriers were identified that hinder the effectiveness of preceptorship within the study institutions. A recurrent challenge was the high student-to-preceptor ratio, compounded by the large number of students from multiple training institutions sharing limited clinical placement sites. This issue of overcrowding is widely reported across Sub-Saharan Africa, where increasing student enrolments in health training institutions have not been matched by proportional growth in clinical teaching capacity [14, 15] Overcrowding in clinical settings limits opportunities for individualized supervision and feedback, thereby constraining experiential learning and compromising the quality of clinical education [16].
Poor communication and coordination between academic institutions and teaching hospitals also emerged as a major barrier. The absence of clear communication channels regarding student placement schedules, learning objectives, and supervision responsibilities often resulted in confusion and inefficiencies. Similar coordination challenges have been documented in other Sub-Saharan African settings, where fragmented relationships between training institutions, and teaching hospitals impede the smooth integration of educational and service delivery goals [17,18,19]. Effective communication is critical in ensuring that students’ clinical experiences are well-structured and aligned with their academic goals [20, 21].
Inadequate preceptorship skills and limited pedagogical training among clinical staff were also reported as significant impediments. Many preceptors lacked formal preparation in educational methods, assessment, and feedback provision skills that are essential for effective clinical teaching. This finding is consistent with evidence from other African contexts, where the absence of structured faculty development programs has been shown to weaken the quality of mentorship and clinical supervision [22,23,24]. Moreover, some preceptors expressed low confidence in their teaching abilities, a challenge similarly noted in studies from Kenya, Tanzania, and Malawi, where limited training and recognition for teaching roles contribute to diminished motivation and performance [25,26,27].
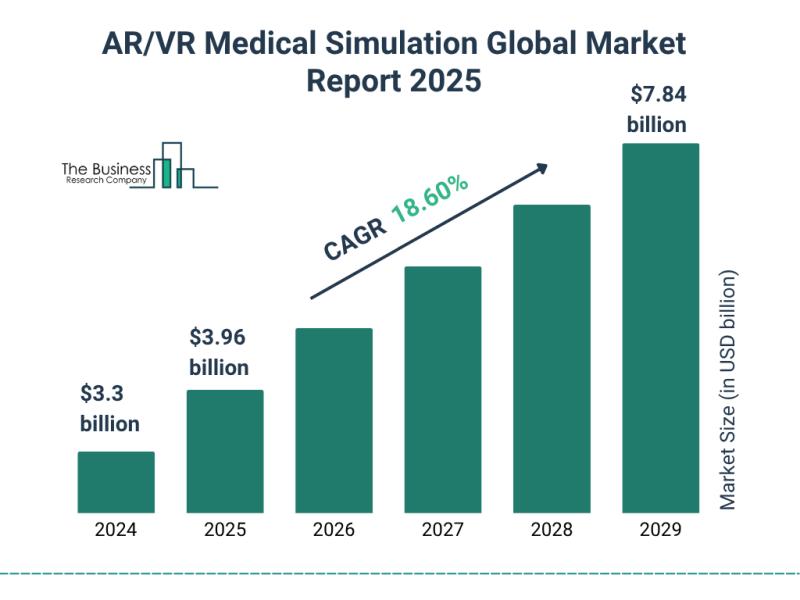
Finally, the shortage of models and equipment in skills labs and simulation lab was a significant barrier, limiting the ability of preceptors to provide hands-on training. The importance of adequate simulation resources in medical and nursing education cannot be overstated, as they allow students to practice and hone their skills in a controlled environment before applying them in real-life scenarios [27, 28]. The absence of such resources, as highlighted in this needs assessment, compromises the effectiveness of clinical teaching and leaves students inadequately prepared for their roles in the healthcare system.
Implications for practice and policy
Our findings have important implications for practice and policy in clinical education. Within low resource settings like Uganda. First, there is a need for enhanced support and capacity-building for preceptors to equip them with the necessary skills and knowledge for effective clinical teaching. Evidence from similar settings in Malawi, Tanzania, and Zimbabwe demonstrates that structured faculty development programs and periodic refresher training in clinical teaching methodologies significantly improve preceptors’ confidence, teaching competence, and student satisfaction [29,30,31].
Addressing the communication gap between academic institutions and hospitals is also critical. Studies in Botswana and Ghana indicated that establishing formal communication frameworks such as joint coordination committees, or clearly defined liaison roles can enhance alignment between academic and clinical partners, improve placement planning, and ensure that learning objectives are consistently met [32, 33]. Furthermore, induction and orientation of students with the health workers at the teaching hospital improves communication and collaboration [34, 35].
Additionally, efforts should be made to manage student numbers in clinical settings to avoid overcrowding, which compromises the quality of education. This could be achieved through phased placements, increasing the number of trained preceptors or increasing the number of health facilities where students do clinical rotation [36]. Finally, a recent meta-analysis in sub-Saharan Africa highlights that investment in simulation labs and skills laboratories is essential equipping students with the practical competencies required before entering the clinical environment [15].
link